Biography
I am an associate professor in the Department of Epidemiology, Biostatistics & Occupational Health at McGill University. I am also a member of the McGill University Centre on Population Dynamics and McGill’s Public Policy and Population Health Observatory. I also hold an endowed chair of Impact of Health and Social Policy on Health Inequalities at Erasmus University Medical Center.
My research focuses on understanding population health and its social distribution, with specific interests in impact evaluation, measuring health inequalities, global health, demography, causal inference, and ethical issues in public health.
More information on specific projects, papers, students, and teaching are in my CV.
- Social Epidemiology
- Impact Evaluation
- Reproducible Research
-
PhD in Epidemiologic Science, 2005
University of Michigan
-
MSPH in Epidemiology, 1999
University of South Carolina
-
BA in Biology, 1995
Westminster College
Media
Twitter timeline
News coverage
- Coverage by The Indian Express and Forbes on our recent paper investigating environmental conditions and suicide in India, 2020-09-19.
- Report by The Leaf News on our paper looking at the cannabis “holiday” on April 20 and fatal traffic crashes, 2019-03-07.
- Feature (and interview) on the Smarter Choices for Better Health Initiative, 2018-11-26.
- Coverage of our paper on gun violence in US states by CNN, 2018-04-23.
- NPR’s Hidden Brain story on our paper looking at the impact of recessions on mortality, 2018-01-16.
- PBS NewsHour coverage of our work on seat belt laws and traffic crash mortality, 2017-04-30.
Projects

Beijing Household Energy Transitions
Health and air pollution impacts of household energy transitions

Tabora Newborn and Maternal Health Initiative
Evaluating a reproductive, maternal and newborn health intervention in Tanzania

Affordable Daycare To Empower Indian Women
Evaluating the impact of daycare on women and children

Antenatal Steroids and Child Health
Assessing the consequences of antenatal corticosteroid administration on child neurodevelopment
Featured Publications
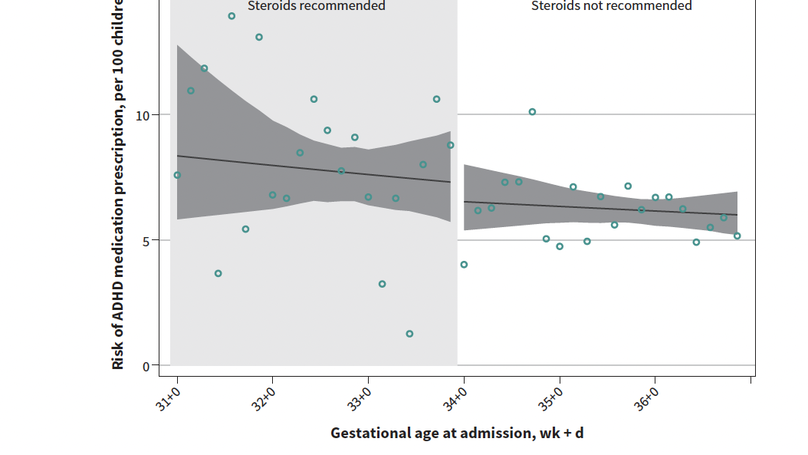
BACKGROUND: Antenatal corticosteroids reduce respiratory morbidity in preterm infants, but their use during late preterm gestation (34-36 weeks) is limited because their safety for longer-term child neurodevelopment is unclear. We sought to determine if fetuses with higher probability of exposure to antenatal corticosteroids had increased rates of prescriptions for attention-deficit/hyperactivity disorder (ADHD) medication in childhood, using a quasiexperimental design that better controls for confounding than existing observational studies. METHODS: We identified 16 358 children whose birthing parents were admitted for delivery between 31 + 0 (31 weeks, 0 days) and 36 + 6 weeks' gestation in 2000-2013, using a perinatal data registry from British Columbia, Canada, and linked their records with population-based child ADHD medication data (2000-2018). We used a regression discontinuity design to capitalize on the fact that pregnancies presenting for delivery immediately before and immediately after the clinical cut-off for antenatal corticosteroid administration of 34 + 0 weeks' gestation have very different levels of exposure to corticosteroids, but are otherwise similar with respect to confounders. RESULTS: Over a median follow-up period of 9 years, 892 (5.5%) children had 1 or more dispensations of ADHD medication. Children whose birthing parents were admitted for delivery just before the corticosteroid clinical cut-off of 34 + 0 weeks' gestation did not appear to be more likely to be prescribed ADHD medication than those admitted just after the cut-off (rate ratio 1.1, 95% confidence interval [CI] 0.8 to 1.6; 1.3 excess cases per 100 children, 95% CI -2.5 to 5.7). INTERPRETATION: We found little evidence that children with higher probability of exposure to antenatal corticosteroids have higher rates of ADHD prescriptions in childhood, supporting the safety of antenatal corticosteroids for this neurodevelopmental outcome.
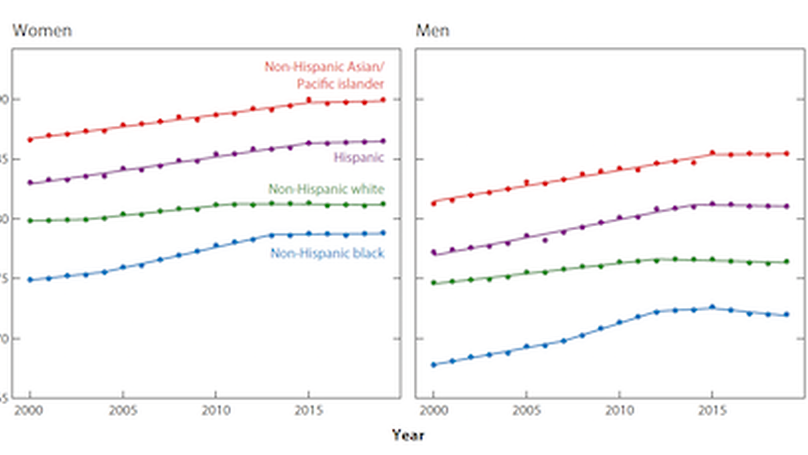
In recent years, life expectancy in the United States has stagnated, followed by three consecutive years of decline. The decline is small in absolute terms but is unprecedented and has generated considerable research interest and theorizing about potential causes. Recent trends show that the decline has affected nearly all race/ethnic and gender groups, and the proximate causes of the decline are increases in opioid overdose deaths, suicide, homicide, and Alzheimer’s disease. A slowdown in the long-term decline in mortality from cardiovascular diseases has also prevented life expectancy from improving further. Although a popular explanation for the decline is the cumulative decline in living standards across generations, recent trends suggest that distinct mechanisms for specific causes of death are more plausible explanations. Interventions to stem the increase in overdose deaths, reduce access to mechanisms that contribute to violent deaths, and decrease cardiovascular risk over the life course are urgently needed to improve mortality in the United States.
Recent Publications
Contact
- sam.harper@mcgill.ca
- +1 514 398 2856
- 1020 Pine Avenue West, Montreal, QC 94305
- By appointment
- DM Me
- Skype Me